When treating plantar fasciitis, some clinicians opt to use a dorsiflexion night splint, which maintains the ankle at a neutral or dorsiflexed position during sleep. Some previous studies suggested that dorsiflexion night splints effectively relieve plantar fasciitis and that their treatment effects were comparable to customized and off-the-shelf foot orthoses . However, some other studies reported that the night splints could easily cause discomfort at the feet and thus lower the quality of sleep and compliance rates and affect treatment outcomes . The discomfort is caused by the high pressure applied from the thermoplastics to the malleolus and the back of the heel when the feet rest on the bed during sleep. Some design changes in improving the comfort of the use of a night splint are required. Further, clinical guidance to employ one stretching over the other is unclear or not well defined.
In a randomized controlled trial, DiGiovanni et al13 compared the efficacy of plantar fascia stretching versus Achilles tendon stretching in a sample of 101 subjects with symptom duration greater than 10 months. In addition to the assigned stretches, all subjects received over the counter prefabricated insoles, three weeks of celecoxib, and a patient educational video. Plantar fascia stretches were performed while sitting and the Achilles tendon while standing by one group, three times a day, for 10 repetitions with a hold of 10 seconds per repetition.
The plantar fascia stretching group also had a higher percentage of positive responses to an outcomes survey in terms of pain, activity and satisfaction. After eight weeks, patients from both groups were instructed to continue with plantar fascia stretching. At two-year follow up,5 both groups continued to show improvement on the pain subscales of the FFI compared to baseline. These two studies suggest that plantar fascia stretches provide better symptom relief for chronic plantar fasciitis.
Our Premium Plantar Fasciitis Brace is designed for those individuals suffering with daytime pain and discomfort associated with Plantar Fasciitis. The Plantar Fasciitis wrap can be used in conjunction in a night splint to help provide both nighttime and daytime relief for Plantar Fasciitis pain and discomfort. According to the Mayo Clinic, heel pain is most commonly caused by inflammation of the plantar fascia--the tissue along the bottom of your foot that connects your heel bone to your toes. For effective treatment while walking or sitting, try this Plantar Fasciitis Daytime Strap Brace.
Fitting comfortably in your shoe, the plantar fasciitis splint features support straps that lift the arch and provide compression to the plantar facia for immediate relief. The compact size our our PF Wrap allows the patient to wear this brace comfortably throughout the day for symptomatic relief. Combine with a Night Splint for around the clock relief for Plantar Fasciitis discomfort. I have shared the pain of you all and besides getting custom orthotics from a reputable podiatrist, I highly recommend you accept the fact that you cannot just wear any type of shoes anymore. To get temporary relief but then continuing to wear shoes that do not give you proper heel and Arch support will be self-defeating.
As far as care when you are not on your feet, for me, calf stretches are a favorite pain reliever and it truly does not take much time to get relief . Even more effective is multitasking with even less effort by doing a light stretch while sleeping! Though they aren't attractive, they are very effective; I am referring to night splints – I encourage calf stretches and wearing a lightweight night splint as often as possible. Some designs available also pull the toes backwards as well as keeping the ankle in a neutral position.
This provides added benefit by stretching the plantar fascia as well as the calve muscles. A night splint is designed to be worn whilst you sleep at night. If you're lucky enough to get a magic 8 hours sleep, this means the night splint is doing all the hard work over a long period of time whilst you enjoy your well deserved rest. When it's time to get out of bed in the morning, you simply take off the splint, put your foot down to the ground, and feel sheer relief that you don't feel as if you've just stood on 50 pieces of Lego. Well this is all well and good in theory, but do night splints actually help plantar fasciitis morning pain?
Records of patients who were treated for plantar fasciitis with either dorsal night splints or adjustable night splints between September 2006 and August 2008 were retrospectively reviewed after obtaining IRB approval. From September 2006 to August 2007, all patients diagnosed with plantar fasciitis by the senior author were placed in a dorsal night splint, enrolled in physical therapy, and given silastic heel cups. From September 2007 to August 2008, all patients diagnosed with plantar fasciitis by the senior author were placed in a traditional adjustable night splint, enrolled in physical therapy, and given silastic heel cups. All patients in both study groups were given the same prescription for formal and home-based eccentric Achilles exercises and stretching, as well as massage, iontophoresis, and ultrasound. If the calf muscles are tight, excessive pronation of the foot may occur to compensate for the reduced ankle dorsiflexion.
This increases the tensile loads on the plantar fascia. The plantar fascia will experience even higher loads if it is tight as well. Dorsiflexing the ankle and the metatarsophalangeal joints during sleep could reduce the tension of the posterior calf muscles and plantar fascia during daytime walking and, therefore, reduce pain.
Poor compliance has been one critical factor affecting the effectiveness of night splints [14–16]. Poor compliance was due to the discomfort and pain caused by overstretching of the calf muscles and the high pressure applied from the thermoplastic component of the splint to the ankle and the back of the heel. The adjustable and soft night splint used in this study addressed these two problems. Subjects could adjust the angle if it created discomfort. In addition, the neoprene material reduced the pressure applied around the ankle and the back of the heel.
A night splint makes the symptoms feel better in the morning after wearing it all night, because the plantar fascia is already stretched before your foot hits the ground first thing in the morning. That means the injury does not re-rip open when you step on it because it has been held open all night. So that means that it can be effective at reducing the pain that people feel first thing in the morning, but it doesn't actually help to heal the problem that is causing the heel pain. If you had a nasty horizontal cut on the back of your elbow and kept your arm straight, you would start to approximate the tissues and it would heal. But every time that you bent your elbow while it was healing, you would feel pain from the cut ripping apart. If you bent your elbow enough then eventually it wouldn't hurt at the cut anymore.
The same thing happens with plantar fasciitis when someone is non-weightbearing for a period of time and then becomes weightbearing. The pain is there while they stretch the plantar fascia out and then once it's been really ripped back open it no longer hurts. Sit for too long and it starts to heal, but once you stand, it hurts. It hurts most in the morning since you have spent so much time non-weightbearing as you sleep. Night splints are a common thing that are recommended fortreatment of plantar fasciitis or plantar fasciosis .
A night splint is a device that is worn while a person sleeps to keep their foot held up in a position like you were walking on your heels. This position is called dorsiflexion and it stretches the calf and Achilles tendon at night. They are commonly recommended by physicians, physical therapists, chiropractic physicians and even podiatrists.
But just because it is a popular or common treatment for heel pain does not mean that it is actually effective1,2. Some organizations have guidelines that recommend night splints to treat plantar fasciitis or Achilles tendonitis. It is true that night splints have been shown to decrease pain in the short term and placate a patient, but that does not mean that it helps long term. For patients who have had difficulties with the use of night splints, a day-wear SAS brace could be another possible option. In addition to the phase of healing, patient's work environment, lifestyle, and the costs associated with treatment should be considered when prescribing a treatment regimen. The patient's compliance with the suggested treatment method should also be monitored and alternative options should be provided.
The most common symptom of plantar fasciitis is morning heel pain. Many sufferers describe the pain as a sharp stabbing or burning pain felt upon those first morning steps. They often turn to heel pads or gel insoles to cushion the area thinking that it is something sharp that needs to be padded. What's actually happening is that the plantar fascia is tearing away from the heel.
The fascia is stretched throughout the day and then contracts and heals in a relaxed position at night. It's similar to having a cut on your knuckle that never heals because the area is constantly being flexed. For many years doctors have prescribed night splints hoping to help relieve the morning pain by stretching the calf.
Calf tightness can predispose someone to develop plantar fasciitis but treating the problem by calf stretching is like washing your hands after you already have a cold. The Strassburg Sock doesn't stretch the calves but flexes the foot without uncomfortably pulling on the toes. This places tension directly on the plantar fascia by taking advantage of something called the Windlass Mechanism. First let's discuss the history of the night splint and how the night splint works to treat the pain associated with plantar fasciitis. Back in the "days of yore" heel pain or plantar fasciitis was frequently treated with immobilization in a walking cast.
This facilitated placing the plantar fascia at rest on a 24/7 basis. The cast also served to re-distribute pressure away from the heel to other structures in the foot, ankle and calf. My first hand research has indicated that the first consistent use of the night splint concept was started at Thomas Jefferson University Medical Center somewhere around 1989 to 1990. The oral history is that Dr. Keith Wapner, yes related to that Judge Wapner, offered a cast to treat the plantar fasciitis of one of his orthopaedic residents.
The resident balked at having to wear a cast thereby leading Dr. Wapner to offer the resident the use of a molded plaster splint that he would wear at night. The morning pain and other pain associated with the resident's plantar fasciitis went adios. However, ultimately Dr. Wapner found that patients did not much like to wear a heavy plaster splint to bed. Sometimes the splint would crack, scratch the other leg or was just too heavy and bulky. This spawned the development of numerous prefabricated splint designs to make a more durable and hopefully more comfortable splint. We will talk about the different types of splint at another time.
The soft neoprene material and the self-adjustable strap tension of the soft night splint could avoid discomfort while maintaining the treatment effects. Another brace option, the night splint, has long been used to treat plantar fasciitis. Several studies38-40 have investigated the effectiveness of the posterior dorsiflexion splint/night splint for the treatment of plantar fasciitis; however most of these studies have yielded mixed reviews. The purpose of the splints is to keep the ankle in neutral position mostly during the night. Although the splints are frequently used for treatment of plantar fasciitis, most of the studies had high dropout rates and low compliance, possibly due to discomfort caused by the splint.
Further, the literature is lacking evidence of superior benefits of the night splint compared to other conventional treatment measures. The treatment of plantar fasciitis aims at affecting the anatomical, biochemical, and environmental factors that may contribute to the development of the condition. Manual passive stretching/active stretching of the Achilles tendon and plantar fascia are the mainstay treatment for plantar fasciitis. Greve et al28 also assessed the effectiveness of combined treatments, including stretching exercises and ultrasound or radial shockwave therapy. Their results suggested that combined treatment of ultrasound and stretching of gastrocnemius and plantar fascia being are as effective as radial shockwave therapy and stretching of the gastrocnemius and plantar fascia. In another study, Hyland et al1 reported a decrease in pain with plantar fascia stretching and calcaneal taping.
In my opinion, the night splint is an incredibly effective device at eliminating heel pain first thing in the morning which is what almost every patient with plantar fasciitis suffers with. I have prescribed many of my patients with night splints and achieved very successful results over the years. It is one of the most readily available, cheap, and effective treatment options for plantar fasciitis as it reduces pain when the patient gets out of bed in the morning. This breaks the pain cycle and promotes faster recovery time from plantar fasciitis. In addition to this, there is moderate quality research evidence to support the use of night splints in the management of plantar fasciitis.
When more conservative managements such as orthotic treatments, stretching exercises, and shockwave therapies are unsuccessful in clinical practice, steroid injection is a preferred option [29–30]. This study provides some clues for improving the treatment outcomes of orthoses, which may prevent subsequently more invasive treatments. Being overweight has been suggested to be a contributing factor to plantar fasciitis, because repetitive and excessive loading can lead to inflammation and consequent pain in the plantar fascia [2–4]. High body weight could deform the PPT material to a larger extent during walking and potentially affect the treatment outcomes.
A previous study indicated that an addition of 9.1 kg of body weight in female subjects increased plantar pressure by more than 10 percent at heel regions . Another study reported that repeated applications of high loading could stiffen insole materials , which could affect their ability to reduce peak pressure. The potential effect of body weight on the function of the foot orthosis was the reason why equal numbers of overweight and normal weight subjects were assigned to the two groups. This study did not further investigate whether the treatment outcome would be worse in an overweight subject group, because such an investigation would largely reduce the statistical power. Because the study spanned 8 weeks, however, ensuring that each subject used the same type of shoes over the entire study period was not feasible. This study used a consecutive sampling approach to include patients who met the inclusion criteria within a certain period of time.
Random sampling, which allows nonprobability biases to be avoided, was not used because this study followed up new incoming patients referred for orthotic treatments. Orthotic insoles and dorsiflexion night splints work in different ways, with insoles reducing the peak plantar pressure and dorsiflexion night splints restoring the flexibility of soft tissues. This led to the hypothesis that combining the use of foot orthoses and night splints might improve pain relief for plantar fasciitis. While the combination approach was used in some clinical centers, the treatment outcomes were not well documented.
The Strassburg Plantar Fasciitis night sock was the first sock proven medically effective for the treatment of plantar fasciitis. The average recovery time in a large, independant research study was 18.5 days with 97.8% of patients recovering within 8 weeks. The Strassburg sock gently holds the toes in place, allowing the foot to flex naturally. This places tension on the plantar fascia without uncomfortably squeezing or stretching the toes and placing unnecessary tension on the calf.
The adjustable toe strap allows the user to increase tension to assist with other injuries where a consistent, controlled stretch may be helpful. In this retrospective study we sought to determine the clinical benefit of applying a dorsal night splint and to compare it to an adjustable night splint in treating plantar fasciitis. In a prospective randomized controlled trial, Porter et al29 randomized 94 subjects to either sustained stretching or intermittent stretching of the Achilles tendon. The sustained stretching group was instructed to stretch for three minutes, three times a day; the intermittent group was instructed to perform five 20-second stretches twice a day. Increased dorsiflexion range of motion correlated with decreased pain and increased function for both groups.
There was no long term follow up and a high dropout rate (29.8%) was observed. The condition's name is derived from the plantar fascia. Plantar fasciitis is an inflammation of the fibrous tissue along the bottom of your foot that connects your heel bone to your toes. Plantar fasciitis is a condition characterized by a stabbing sensation in the heel that most often accompanies your first steps of the day. Once you have moved around a bit, limbering up your foot, the pain typically eases.
Similarly, the stabbing sensation may also flare up when you stand after sitting for an extended time. The pain may also return following long hours on your feet or after an intense bout of physical activity. The main function of the orthotic insoles used in this study was to reduce the peak pressure under the heel , because the elastic insole material deforms at each walking step, increasing the contact area with the foot .
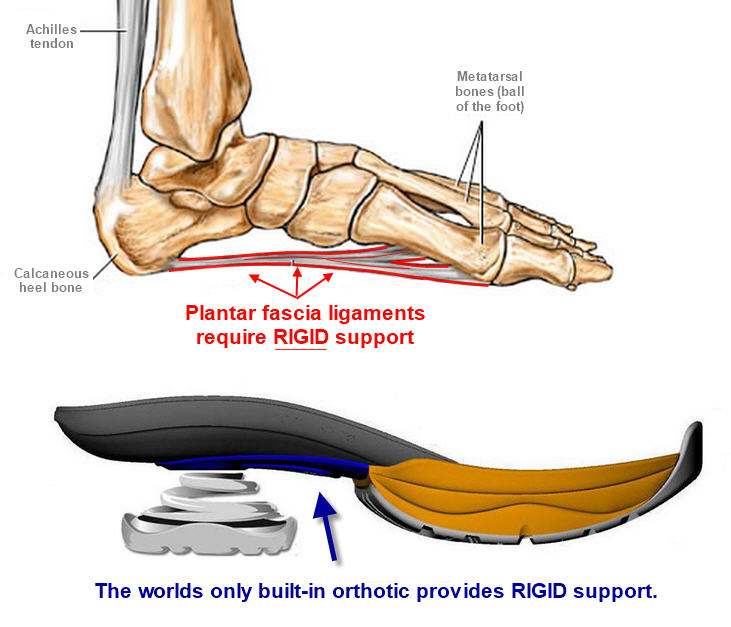
These orthoses did not require casting of the foot, which reduced the manpower and time of an orthotist and, therefore, reduced production cost. Such orthoses could realign the foot during weight bearing by providing appropriate arch supports. A previous study suggested that both types of insoles effectively reduced pain scores in 4 weeks . In our study, the accommodative orthotic insole lowered mean pain scores over the 8 weeks; however, a statistical difference was not found. Significant reductions in pain and total FFI scores were achieved when combining the orthotic insole with the self-adjustable night splint. Plantar fasciitis is a condition that involves the inflammation of the plantar fascia .